|
Miriam Bauwens defended successfully her PhD thesis on "Missing heritability in ABCA4-associated disease" on the 19th of September 2018 in Ghent. Congratulations Miriam!
Check out our latest paper published in Genetics in Medicine. You can read the abstract below, for the full text click here.
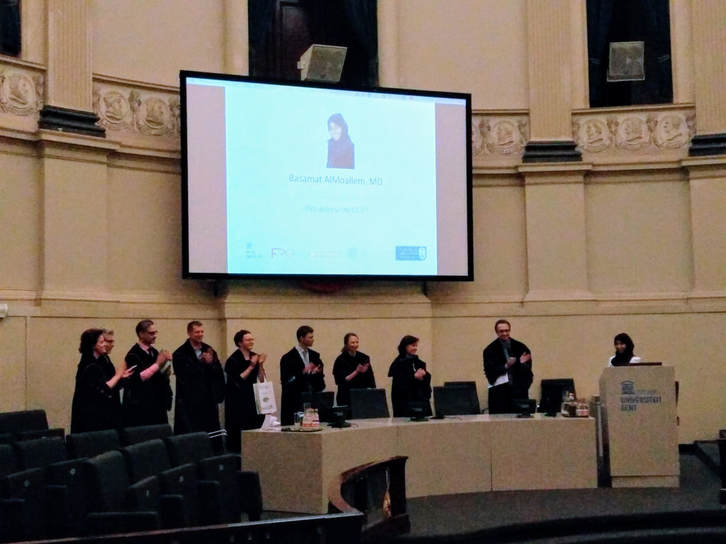
Purpose: Disorders or differences of sex development (DSDs) are rare congenital conditions characterized by atypical sex development. Despite advances in genomic technologies, the molecular cause remains unknown in 50% of cases. Methods: Homozygosity mapping and whole-exome sequencing revealed an ESR2 variant in an individual with syndromic 46,XY DSD. Additional cases with 46,XY DSD underwent whole-exome sequencing and targeted next-generation sequencing of ESR2. Functional characterization of the identified variants included luciferase assays and protein structure analysis. Gonadal ESR2 expression was assessed in human embryonic data sets and immunostaining of estrogen receptor-β (ER-β) was performed in an 8-week-old human male embryo. Results: We identified a homozygous ESR2 variant, c.541_543del p.(Asn181del), located in the highly conserved DNA-binding domain of ER-β, in an individual with syndromic 46,XY DSD. Two additional heterozygous missense variants, c.251G>T p.(Gly84Val) and c.1277T>G p.(Leu426Arg), located in the N-terminus and the ligand-binding domain of ER-β, were found in unrelated, nonsyndromic 46,XY DSD cases. Significantly increased transcriptional activation and an impact on protein conformation were shown for the p.(Asn181del) and p.(Leu426Arg) variants. Testicular ESR2 expression was previously documented and ER-β immunostaining was positive in the developing intestine and eyes. Conclusion: Our study supports a role for ESR2 as a novel candidate gene for 46,XY DSD. On Friday December 8 2017 Basamat ALMOALLEM, a Saudi ophthalmologist in training, successfully obtained her PhD in Health Sciences on the basis of her doctoral thesis ‘Unraveling the molecular basis of genetically heterogeneous developmental eye disorders’. Her findings unveiled examples of care valued by both patients and clinicians in the field of ophthalmic genetics. She has taken great steps towards tackling some of the challenges ophthalmic genetics is facing today.
For our new team website we obviously needed a nice team picture. The crime scene of choice was the historic centre of Ghent. We would like to thank our photographer Pieter-Jan Volders for the beautiful photos. In the picture below you can see the models getting ready for the shoot.
|
De Baere Lab © 2024